Article begins
It never once occurred to me, during the six years I conducted research on racism, pregnancy, and premature birth, that the birth stories people shared would—or could—be translated into visual form. Illustrating racism and adverse birth outcomes is complicated by, among other things, the ethnographic research mandate of anonymity and the use of pseudonyms, citations, footnotes, and theoretical references. But something about illustration breathes a different kind of life and knowingness into that mandate.
How does one tell a birth story or stories that bear the burden of racism? As an anthropologist who deploys and writes ethnography I often ask, What can ethnography accomplish? This collaboration is an effort in disobedience against the “typical” academic form. Sharing a birth story of obstetric racism, any story really, accompanied by illustrations and poetry is one way in which people who live in the world uninvited, are able to enter a world with witnesses, with others, with other senses—the heart, the eyes, and the ears.
These factors make this birth story different because the person from whom the story originates wanted it to be known. LeConté is her name and she shared her birth story and her poem with intention because she understands the power of reconstituting oneself after having experienced racism.
Collaborating with LeConté along with birth worker and graphic designer, Cheyenne Varner, constitutes a kind of recovery of the pieces of Black women’s lives that are lost as a result of obstetric racism. Cheyenne, for her part, understands the importance of representing Black women’s images and stories. There is power in having our stories communicated in a variety of ways and the power of sharing their stories is fundamental. It is one thing to hold your story in your memory, but it another thing to hear it and still another to see it illustrated. Each of these elements carry power because part of telling and illustrating someone’s birth story is the fact that they are at center. In an environment where some Black women feel marginalized—that is medical spaces—LeConté, Cheyenne, and I have collectively moved one Black woman’s experience of her medical encounter from the margin to the center.

LeConté is a 40-year-old Black professional who had in vitro fertilization (IVF). When she found out she had conceived, she was ecstatic and set about developing her birth plan. She and her husband agreed they wanted little to no interventions. She wanted a vaginal birth. Over the course of several months the two of them prepared for the arrival of the baby. They developed a birth support team that included two doulas, one of whom was me. One of her doulas knew some of the nurse midwives at the hospital where LeConté planned to give birth. Arrangements were made for those nurse midwives, who were Black and possessed the most politically informed analysis of Black women’s birthing experiences, to be on call when LeConté was admitted. Her obstetrics-gynecology (OB-GYN) team comprised two female doctors, one of whom was Black.
At my suggestion, LeConté and her husband engaged in several projects that they viewed as radical caring. They created a collage vision board of the kind of labor and birth they wanted and it helped to center LeConté’s focus during labor. The couple also wrote letters to their baby about what they wished for her and to each other. I also suggested that they gift each other aromatherapy scents they each found calming and could be used during the labor.
The pregnancy proceeded well until LeConté was 35 weeks. When LeConté went for a prenatal check-up her blood pressure reading was 147/81, which led to a diagnosis of severe preeclampsia. A second blood pressure reading that same day was 135/83. But it was the result of the test for her liver enzymes that caused alarm. There was protein in her urine. The next day, after the test results came back, LeConté’s OB-GYN team instructed her to go to the hospital for admission. They wanted to induce labor.

LeConté’s support team went to the hospital with her. She arrived with her husband, her mother, and two doulas. They had a playlist, an exercise ball, the collage, and their birth plan.
LeConté’s doctors were committed to LeConté having a vaginal birth and closely monitored her blood pressure, which was normal the entire labor although her liver enzymes were four times higher than normal. If both had been elevated, she would have needed a C-section. The absence of high blood pressure meant that she could possibly have a vaginal birth.
Over two days, LeConté’s labor was induced. A fetal monitor restricted her movement. A supportive team of nurse midwives attended to LeConté. But there were some issues along the way. When a nurse came in to insert the IV, she was unable to find a vein. She poked and poked and poked. LeConté winced in pain. It was like the nurse was unaware of how much pain she was causing. And even when she knew, she did not stop poking.
At one point, one of the nurses did a blood draw, and when some of the blood squirted near the air conditioning unit the nurse did not clean it up until LeConté asked her to do so. Then the nurse lost one of the vials of blood.
Labor induction began with LeConté receiving an epidural. But the anesthesiologist who came to her room administered too much epidural, causing her to feel dizzy. Annoyed that he had to come down to the labor and delivery unit, he commented to one of the doctors, in front of LeConté and everyone in the room, “Why don’t you just give her a C-section? I am not coming down here again.” LeConté felt invisible and disrespected.
LeConté’s doctors also told her that the quality improvement person on duty wanted her to have a C-section. Black women are more likely to have C-sections than any other group of women, according to the Centers for Disease Control and Prevention. It seemed that there were powerful forces conspiring to prevent LeConté from having a vaginal birth and to LeConté it also felt like a race-based decision.
But her doctors were convinced that with labor induction using Pitocin and a Foley bulb induction, LeConté could have a vaginal birth. They fought the fight for her against the force of the medical complex.

In the afternoon of LeConté’s second day at the hospital, a beautiful little girl arrived. But at midnight, LeConté was transferred to the postpartum floor. No wheelchair was provided and she had to walk to another room, pushing her newborn in the mobile crib and her IV, with her husband trailing behind her, carrying all of their belongings.
LeConté cried. She wanted to break out of the hospital. She wanted to be a mother in her own home, not in the hospital where they poked and prodded her. This is the poem she wrote about her experience.
MOVING TO THE POSTPARTUM FLOOR
Feels like a demotion
Feels like I did something wrong
No longer are they waiting on me
on hand
and foot
step careful
cautious
It’s midnight and
they made me push my baby
new
born just yesterday
Don’t look behind me
but I know hubby’s there
carrying 10,000 bags
what in the bootleg nativity
is this
new room has a neighbor
mommy and baby behind a curtain
her baby
sleep my baby
up my baby
sleep her baby
up every couple hours
to feed
to take a new test
night nurses not nice nurses
press my breasts hard
press my arms hard
begging for my milk and my blood
such sacrifice
I want to go home
Want to go make a home
Hospitals are not homes
In the meantime, I search for Google images of 2Pac
breaking out of Bellevue
It’s right down the street
But feels boroughs away
Anyway, Pac knew a hospital is not a home
I, too, plot our escape
or dream of a baby’s Uber ride
or freak out about baby girl’s first Uber ride
or dream about home
apartment
box
in Brooklyn
and the mother who I will grow into being
there
LeConté Dill
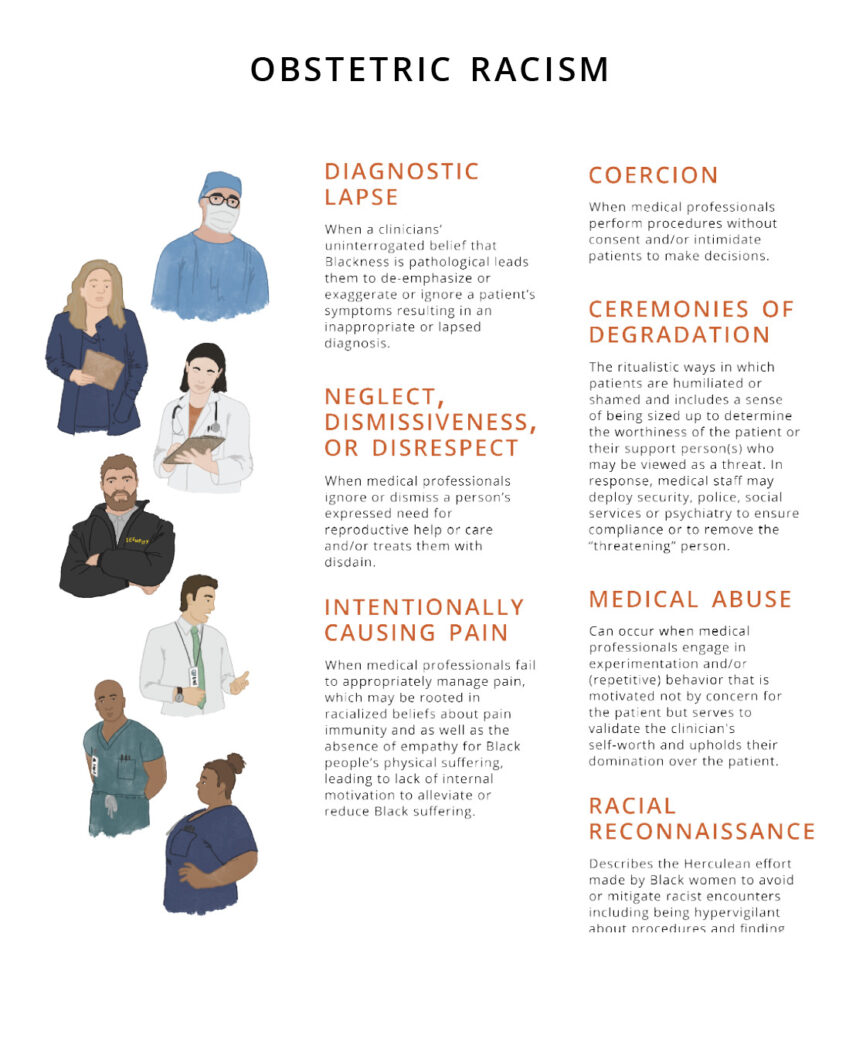
LeConté experienced what she believed and felt was racism, what I call obstetric racism. Obstetric racism sits at the intersection of obstetric violence and medical racism. It is the mechanisms and practices of subordination to which Black women and people’s reproduction are subjected that track along histories of anti-Black racism during preconception, pregnancy, prenatal care, labor, birth, and postpartum care. It characterizes situations when obstetric patients experience reproductive dominance by medical professionals and staff compounded by a patient’s race or the history of racial beliefs that influences the treatment or diagnostic decisions. There are seven dimensions of obstetric racism: diagnostic lapses; neglect, dismissiveness, or disrespect; intentionally causing pain; coercion; ceremonies of degradation; medical abuse; and racial reconnaissance.
Although experiences can be overlapping, of the seven dimensions, LeConté experienced at least three. When the anesthesiologist made LeConté feel invisible and disrespected, that exemplified neglect, dismissiveness, or disrespect. The nurse’s repeated attempts to insert the IV was painful, but despite LeConté telling her it hurt, the nurse continued, which amounted to intentionally causing pain. One might argue that making LeConté walk to the postpartum unit several hours after giving birth and pushing both her newborn and her IV was a form of humiliation, a ceremony of degradation.
Although LeConté was induced and her daughter born four weeks early, she was functionally mature and did not require admission to the neonatal intensive care unit. While the outcome appears to be a good one because LeConté had a vaginal birth and her daughter was born healthy, her assessment of the process of her labor contradicts what some may view as a favorable outcome. Hers is a story of obstetric racism.
Obstetric Racism
Diagnostic lapses
When a clinician’s uninterrogated belief that Blackness is pathological leads them to de-emphasize, exaggerate, or ignore a patient’s symptoms, resulting in an inappropriate or lapsed diagnosis.
Neglect, dismissiveness, or disrespect
When medical professionals do not pay attention to a person in need of reproductive care or treat them with disdain.
Intentionally causing pain
When medical professionals fail to appropriately manage pain, which may be rooted in racialized beliefs about pain immunity and the absence of empathy for Black people’s physical suffering, leading to lack of internal motivation to alleviate or reduce Black suffering.
Coercion
When medical professionals perform procedures without consent or intimidate patients to make decisions, such as telling a patient their baby will be harmed if they don’t have a particular procedure.
Ceremonies of degradation
The ritualistic ways in which patients are humiliated or shamed and includes a sense of being sized up to determine the worthiness of the patient or their support person(s) who may be viewed as a threat. In response, medical staff may deploy security, police, social services, or psychiatry to ensure compliance or to remove the “threatening” person.
Medical abuse
Can occur when medical professionals engage in experimentation or repetitive behavior that is motivated not by concern for the patient but serves to validate the clinician’s self-worth and upholds their domination over the patient.
Racial reconnaissance
Describes the Herculean effort that Black women make to avoid or mitigate racist encounters, including being hypervigilant about procedures and finding providers.

